Contact Information
| Telephone: | (852) 2255 2208 |
| Fax: | (852) 2819 3780 |
Scope and Service
The Division of Head and Neck Surgery is dedicated to deliver the highest standard of care for patients with cancer of the head and neck.
The head and neck surgical team comprises of experts in the field of otorhinolaryngology, plastic and reconstructive surgery who specialize in head and neck tumor extirpation and reconstruction. The specialists in the team work together and have over the years built up a reputation of a tertiary referral center, not only for Hong Kong, but also for Asia and internationally.
Via an interdisciplinary approach, experts from across disciplines come together to provide state-of-the-art care for all types and stages of head and neck tumors, specifically tailored to address the needs of individual patient. Treatment may include surgery, radiation therapy, chemotherapy, or a combination of therapies. Comprehensive treatment plans are designed to provide the highest level of care and to optimize functional outcome.
Skull Base Tumour
Tumors in the base of skull e.g. olfactory neuroblastoma, paranasal sinus malignancy, can be resected by endoscopic approach or combined cranio-facial / cranio-nasal approach.
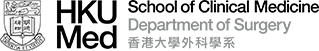
Recurrent Nasopharygneal Tumour
Nasopharyngectomy for local recurrence
- Robot assisted approach
- Endoscopic approach
- Maxillary swing approach
- Combined cranio-facial approach
- Extra-cranial intra-cranial bypass surgery
Neck dissection for neck recurrence
- Brachytherapy
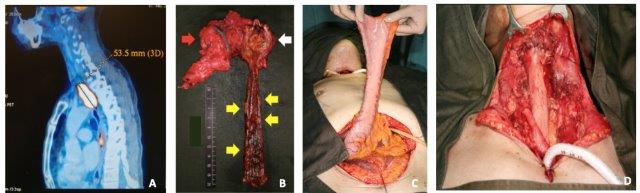
ILLUSTRATION
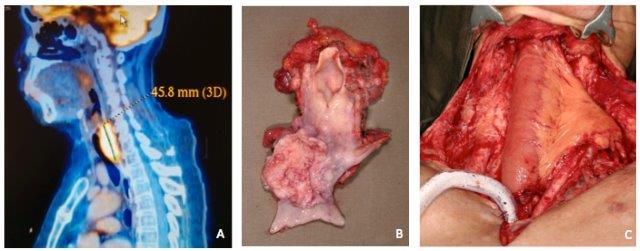
1. Trans-oral robotic nasopharyngectomy.
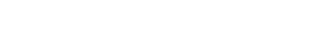
2. Recurrent nasopharyngeal tumor with encasement of left internal carotid artery (A) requiring extra-cranial intra-cranial bypass with radial artery graft (B) prior to nasopharyngectomy.
Oral Cavity & Laryngo-Pharygneal Tumour
Tumors in the oral cavity, oropharynx, larynx, hypopharynx and cervical oesophagus can be resected transorally and/or transcervically
- Robot assisted approach
- Endoscopic approach
- Manubrial resection
- Pharyngo-laryngo-cervico-oesophagectomy (PLCO)
- Total pharyngo-laryngo-oesophagectomy (PLO)
Choice of reconstruction include:
- Pectoralis Major flap
- Deltopectoral flap
- Lateral thoracic flap
- Jejunum
- Radial forearm
- Anterolateral thigh
- Rectus abdominis
- Latissimus dorsi
- Fibular osseocutaneous
Pedicled flaps
Microvascular free flaps
ILLUSTRATION
1. Work-horse flaps in head and neck reconstruction.
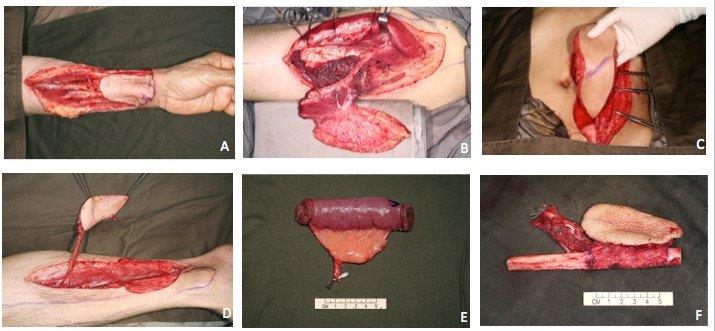
A. Radial forearm flap B. Anterolateral thigh flap C. Vertical rectus abdominis flap D. Posterior tibial flap E. Jejunal flap F. Fibular flap.
2. Oral cavity tumour – resection and reconstruction.
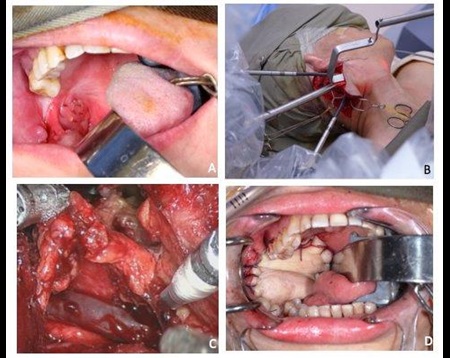
A. Right retromolar trigone acinic cell carcinoma. B. Side-docking of robotic arms via post-auricular posterior hairline incision. C. Robot assisted right neck dissection. D. Free posterior tibial flap for reconstruction of intra-oral mucosal defect.
3. 3D Printing in mandibular reconstruction.
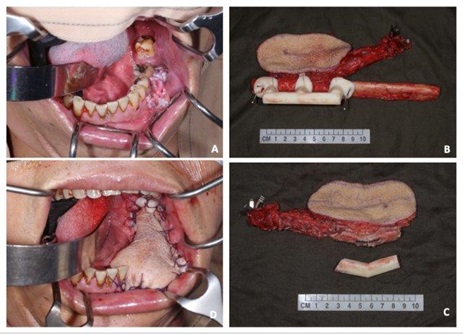
A. Carcinoma of left lower alveolus. B&C. Reconstruction using free fibula osseocutaneous flap. 3D printing was used to optimize bony contour and alignment. D. Skin island used to reconstruct intra-oral mucosal defect.
4. Pharyngo-laryngo-cervico-oesophagectomy (PLCO).
A. Isolated pharyngo-oesophageal tumor. B. PLCO specimen. C. Reconstruction with free jejunal flap.
5. Total pharyngo-laryngo-oesophagectomy (PLO) and gastric pull-up.
A. Pharyngo-oesophageal tumour and synchronous tumours in the lower oesophagus. B. PLO specimen. C. Gastric pull up. D. Pharyngo-gastric anastomosis in the neck.
Experience 1966-2010: 362 PLO and gastric pull-up.
Salivary Gland Tumour
- Robot assisted approach
- Endoscopic approach
- Conventional open approach
ILLUSTRATION
1. Robot assisted submandibular sialoadenectomy.
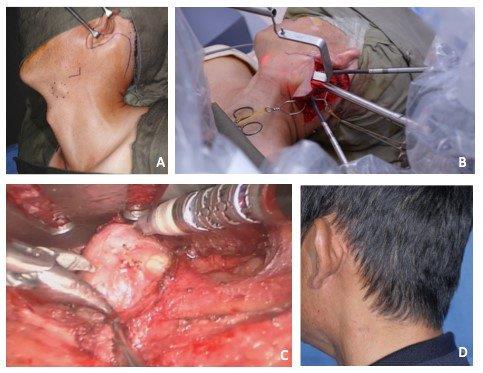
A. Left submandibular gland pleomorphic adenoma. B. Side-docking of robotic arms via posterior hairline incision. C. Robot assisted left submandibular sialoadenectomy. D. Inconspicuous scar 1 year post operation.
Other Challenging Head and Neck Tumours
- Carotid body tumor
- Cranial nerve schwannoma
- Sarcoma
- Parapharyngeal space tumor
- Recurrent tumor
Research
Staff of the Division actively participate in both clinical and laboratory research. Some of our current research interests include the following:
- Anatomical and physiological studies of free jejunum flap
- Management of recurrent pharyngo-oesophageal tumors
- The application of PET-CT scan and plasma EBV-DNA level in patients with recurrent nasopharyngeal carcinoma
- Various approaches in the management of recurrent nasopharyngeal carcinoma
- The use of narrow band imaging in the surveillance of Head and Neck cancer
- Genetic and epigenetic alterations of head and neck cancers
- Gene polymorphism and risk of recurrent nasopharyngeal carcinomas
- Molecular cancer detection with DNA, RNA, and micro-RNA markers
- Cancer stem cells and chemoresistance
- Epstein-Barr virus activities in undifferentiated nasopharyngeal carcinomas
- Use of natural polyphenols in cancer prevention and treatment
- Epigenetic alterations in laryngeal carcinomas
Recent Publications
- Tracheostomy during COVID-19 pandemic – a novel approach.
Chow VL, Chan JY, Ho VW, Pang SS, Lee GC, Wong MM, Lo AS, Lui F, Poon CC, Wong TS.
Head Neck. 2020 May 1. doi: 10.1002/hed.26234. Online ahead of print. PMID: 32358855.
- Novel approach to reduce SARS-CoV-2 transmission during trans-oral robotic surgery
Chow L.Y.V., Chan Y.W., Wong M.M.K., Wong T.S. and Tsang R.K.Y.
Journal of Robotic Surgery.2021, 1-8.
- Conservation of personal protective equipment for head and neck cancer surgery during COVID-19 pandemic.
Chow VL, Chan JY, Ho VW, Lee GC, Wong MM, Wong TS, Gao W.
Head Neck. 2020 Apr 28. doi: 10.1002/hed.26215. Online ahead of print. PMID: 32342543.
- Indocyanine green and Firefly for real-time sentinel lymph node mapping in oral cavity cancer.
Chow VL, Chan JY, Ng JC, Tsang RK.
Surg Oncol. 2020 Mar;32:88-89.
- Swallowing disorders following free jejunal flap reconstruction of circumferential pharyngeal defect: Does Botox help?
Chow VL, Chan JY, Cheng IK, Chan KM.
Oral Oncol. 2020 Mar 2;104:104612. Doi:10.1016/j.oraloncology.2020.104612.
- Esophago-gastric preservation in the surgical management of proximal esophageal cancer.
Chow VL, Chan JY, Law SY.
Ann Thorac Surg. 2019 Jun 7. pii: S0003-4975(19)30738-6. doi: 10.1016/j.athoracsur.2019.04.060. [Epub ahead of print]
- Transoral robotic total laryngopharyngectomy and free jejunal flap reconstruction for hypopharyngeal cancer.
Chan JY, Chan RC, Chow VL, Tsang RK, Wong ST, Wei WI.
Oral Oncol. 2017 Sep;72:194-196. doi: 10.1016/j.oraloncology.2017.06.028. Epub 2017 Jul 15.
- Salvage surgery for recurrent carcinoma of the cervical esophagus postesophagectomy.
Chow VL, Chan JY, Wei WI.
Head Neck. 2015 Aug;37(8):1170-5. doi: 10.1002/hed.23730. Epub 2014 Jul 11.
- Reconstruction of circumferential pharyngeal defects after tumor resection: reference or preference.
Chan JY, Ng RW, Liu LH, Chung HP, Wei WI.
J Plast Reconstr Aesthet Surg. 2011 Aug;64(8):1022-8. doi: 10.1016/j.bjps.2011.03.021. Epub 2011 Apr 11.
- Manubrial resection and anterior mediastinal tracheostomy: friend or Foe?
Chan JY, Chow VL, Liu LH, Wei WI.
Laryngoscope. 2011 Jul;121(7):1441-5. doi: 10.1002/lary.21852. Epub 2011 May 18.
- Surgical salvage of recurrent nasopharyngeal carcinoma.
Chan JY.
Curr Oncol Rep. 2015 Mar;17(3):433. doi: 10.1007/s11912-014-0433-x.
- Extracranial/intracranial vascular bypass and craniofacial resection: New hope for patients with locally advanced recurrent nasopharyngeal carcinoma.
Chan JY, Wong ST, Chan RC, Wei WI.
Head Neck. 2016 Apr;38 Suppl 1:E1404-12. doi: 10.1002/hed.24234. Epub 2015 Nov 13.
- Surgical salvage for recurrent retropharyngeal lymph node metastasis in nasopharyngeal carcinoma.
Chan JY, Chow VL, Wong ST, Wei WI.
Head Neck. 2013 Dec;35(12):1726-31. doi: 10.1002/hed.23214. Epub 2013 Mar 6.
- Indocyanine green fluorescence mapping of sentinel lymph node in patients with recurrent nasopharyngeal carcinoma after previous radiotherapy.
Chan JY, Tsang RK, Wong ST, Wei WI.
Head Neck. 2015 Dec;37(12):E169-73. doi: 10.1002/hed.24052. Epub 2015 Jul 14.
- The role of Epstein-Barr virus-encoded microRNA BART7 status of resection margins in the prediction of local recurrence after salvage nasopharyngectomy for recurrent nasopharyngeal carcinoma.
Chan JY, Wong ST, Wei WI.
Cancer. 2015 Jul 15;121(14):2358-66. doi: 10.1002/cncr.29380. Epub 2015 May 8.
Training
The Division of Head and Neck Surgery offers opportunities for local and international fellows and students to attach and learn with the team. Globally-renowned professors are invited to give lectures from time to time. Various courses, including cadaveric and animal dissection workshops, are regularly organized. We have also been organizing Head and Neck Courses annually over the past 2 decades.
- Local
- International
- Global Online Fellowship (GOLF) in head and neck surgery and oncology, International Federation of Head and Neck Oncologic Societies (IFHNOS)
- Education
- Head and Neck Course in Hong Kong
| Year | Past courses |
|---|---|
| 1994 | Pectoralis major myocutaneous flap |
| 1995 | Micro-vascular free flaps |
| 1996 | Hypopharyngeal cancer |
| 1997 | Intraoral tumour |
| 1998 | Skull base and nasopharyngectomy |
| 1999 | Prevention and management of complications in head & neck surgery |
| 2000 | Neck mass and neck dissection |
| 2001 | Advanced techniques |
| 2002 | Thyroid and Salivary Gland |
| 2003 | Suspended due to SARS |
| 2004 | Cutaneous lesions and soft tissue tumors |
| 2005 | Pedicled flaps (live surgery) |
| 2006 | Microvascular free flaps (live surgery) |
| 2007 | Surgery for Nasopharyngeal Cancer (live surgery) |
| 2008 | Recurrent Head & Neck Tumours (live surgery) |
| 2009 | Neck mass (live surgery) |
| 2010 | Palliative Therapy for Head and Neck Cancer (live surgery) |
| 2011 | Common Intraoral Pathologies (live surgery) |
| 2012 | Cancer of the Larynx and Hypopharynx |
| 2013 | Cancer of the Paranasal Sinuses |
| 2014 | Nasopharyngeal carcinoma |
| 2015 | Practical approaches to head and neck reconstruction (Live surgery) |
| 2016 | Management of salivary gland tumors (Live surgery) |
| 2017 | Recent advances in head and neck surgery (Live surgery) |
| 2018 | Management of recurrent head and neck tumors (Live surgery) |
| 2019 | Prevention and management of complications in head and neck cancer surgery (Live surgery) |
| 2020 | Suspended due to the COVID-19 pandemic |
| 2021 | Head and neck robotic surgery |
| Year | Past courses |
|---|---|
| 2022 | Innovations and survivorship |
| 2023 | Prevention and management of complications |
- International Comprehensive Head and Neck Course
| Year | Country |
|---|---|
| 1997 | Changchun, China |
| 1998 | Changchun, China |
| 1999 | Beijing, China |
| 2000 | Tianjin, China |
| 2001 | Chengdu, China |
| 2002 | Wuhan, China |
| 2003 | Jiangxi, China |
| 2004 | Guizhou, China |
| 2005 | Shanghai, China |
| 2006 | Chongqing, China |
| 2007 | Changsha, China |
| 2008 | Qingdao, China |
| 2009 | Xi'an, China |
| 2011 | Qinghai, China |
| 2012 | Hefei, China |
Clinical Session
Outpatient consultations are provided every Tuesday pm, on the 4th floor, Block S, Queen Mary Hospital. Private patients are seen on the 1st floor, Block J, Queen Mary Hospital by appointment.
Head and Neck Surgery
Division Chief
Dr. Velda Ling-Yu CHOW 周令宇
Consultant
Honorary Clinical Associate Professor
- MBBS(HK), MS(HK), MRCSEd, FCSHK, FHKAM(Surgery)
| (852) 2255 2208 | |
| cly329@ha.org.hk | |
| Publications |
Staff List
| Name | Title | Position | Staff types | Telephone | |
|---|---|---|---|---|---|
| Dr. Jimmy Yu-Wai CHAN 陳汝威 |
Division member | Clinical Associate Professor (Part-time) | Academic staff | (852) 2255 2208 | jywchan1@hku.hk |
| Dr. Valerie Wai-Yee HO 何惠儀 |
Division member | Associate Consultant | Hospital Authority staff | (852) 2255 2208 | --- |