Francis Y.H. Tien Vascular Centre
Management of Vascular Diseases
Abdominal Aortic Aneurysm
Abdominal aortic aneurysm (AAA) is an abnormal dilatation of the abdominal aorta that occurs when a weakening of the aortic wall causes it to expand. AAA is usually asymptomatic, though pulsatile abdominal mass may sometimes be noted by the patient. The main concern is its potential of rupture, which is rapidly fatal. In general, the risk of rupture is related to the aneurysm size and this risk increases dramatically for aneurysms greater than 5 cm in diameter. Therefore, in general, AAA over 5 cm in diameter should be repaired electively in patients who are otherwise good surgical candidates. The operative mortality rate for elective AAA repair is less than 5 %, while the risk of emergency repair for ruptured AAA well exceeds 50 %.
Traditionally, AAA repair is done by open surgery where the diseased segment of abdominal aorta is replaced with a synthetic graft. Recently, endovascular repair involving the placement of an endoluminal stent graft emerged as an alternative form of treatment. Endoluminal stent graft is performed via two small vertical incisions over both groins, whereas traditional open surgery requires a major laparotomy. It offers the advantage of a less invasive procedure and a decreased risk of major morbidity, though its long-term efficacy remains to be assessed. In particular, regular follow up with computed tomography is vital for endoluminal stent graft in order to look for evidence of endoleak which may need further intervention.

CT angiography with 3D reconstruction of thoracoabdominal aortic aneurysm pre- and post- endovascular repair.
Aortic dissection
Aortic dissection is a catastrophic emergency often affecting patient with hypertension. It involves separation and splitting of the layers of aortic wall by blood and leads to sudden chest pain and abdominal pain and with a significant mortality from the aortic rupture, heart valve incompetence, and branch occlusion leading to stroke. Lesser squeal includes kidney failure, and visceral and lower limb ischemia. Traditional surgical repair is a major undertaking and involves split sternum, cardiopulmonary bypass, and graft and valve replacement. It carries morality exceeding 10% and significant morbidity. Survival estimates were 60% at five years. Chronic complications such as late dilatation of the aorta and aneurysm formation also added to a poor long term morbidity and mortality from subsequent operations.
Endovascular repair of aortic dissection is a new treatment involving the placement of a stent graft across the entry tear, with an aim to alleviate pain, limits further dissection and prevents complications and aneurysm formation. Branch vessels that are compromised by the high pressure false lumen will usually realign with reprefusion via the true lumen. Id is an attractive minimally invasive alternative which avoids the high risk and expensive open chest surgery and cardiopulmonary bypass. This procedure also ensures a low morbidity and short hospital stay, less blood loss and quicker recovery. It is particularly suitable for the elderly and the sick and is fast becoming the standard of treatment of aortic dissections.
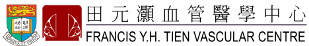
Carotid Stenosis
The carotid arteries are the major blood vessels that carry blood from the heart to the brain and other parts of the head. As people age, the blood flow through one or both of the carotid arteries can be blocked due to atherosclerosis plaques. Stroke may then occur because of this blockage. In some patients, surgery to remove the plaque may be an effective treatment to reduce the risk of stroke. This surgery is called carotid endarterectomy.
Carotid endarterectomy is done in an operating theatre. After making an incision in the neck, the surgeon exposes the common carotid artery, and the area at which it divides into the internal carotid artery and the external carotid artery. All of the plaque causing the stenosis in the area of the surgery will be removed. Carotid endarterectomy usually takes about two or three hours.
Landmark studies have provided convincing evidence on the benefits of carotid endarterectomy in both symptomatic as well as asymptomatic patients with significant carotid stenosis. The operative mortality/stroke rate in asymptomatic patients is less than 3 %, while that in symptomatic patients is less than 6 %.
Carotid angioplasty has been introduced recently as an alternative approach to open surgery, though its safety and long term efficacy remains to be proven. It offers an alternative treatment for patients who are of higher surgical risk either due to their poor medical conditions or due to the unfavourable anatomy of the lesions.
A severe stenosis in the internal carotid artery (ICA). The ICA is one of the main arteries that feeds the eyes and parts of the cerebral hemispheres. Scarce supply of blood to these areas may lead to strokes.
Atheroslcerotic Occlusive Disease
The arteries supplying the lower extremities may be narrowed in a process called atherosclerosis. This is especially pronounced in patients with risk factors like smoking, hypercholesterolaemia, diabetes mellitus and hypertension.
Blood flow to the extremities may be reduced because of this narrowing, and may not adequately provide for the need of oxygen for the tissues. Many patients experience leg pain, referred to as "intermittent claudication". It is a pain in the leg muscles that develop during exercise, when demand for oxygen is high and supply of blood is low. At this stage, the discomfort can be quickly alleviated by rest. If the blood supply is further limited, rest pain or tissue loss ensues.
Treatment includes medical treatment with anti-platelet agent, together with control of risk factors. Good foot care and proper foot wear are also important. In patients with disabling intermittent claudication or those with advanced ischaemia with rest pain or tissue loss, surgery would be recommended.

A gangrene toe. If atherosclerotic occlusive disease in the lower limb is left untreated, tissues may die due to a lack of oxygen supply.
Chronic Venous Insufficiency
Chronic venous insufficiency (CVI) is a common disease with significant socio-economic consequences. It is estimated that 1 to 3 % of adults will develop CVI and about 1.5 % will experience a venous stasis ulcer during their lives. Patients may present with various degree of CVI, ranging from venules, varicose veins, to those with advanced CVI with skin changes like lipodermatosclerosis or venous ulceration.
Both superficial veins and deep veins are responsible for transporting deoxygenated blood from the legs to the heart. The direction of the blood flow is directed by valves in the veins and muscles around them. Veins may become incompetent due to inherent weakness of venous walls or congenital absence of venous valves. The veins may also enlarge, losing competence, following pregnancy or valve damage by blood clots. As a result of this incompetence, blood no longer travels back to the heart efficiently. Over time, the chronically elevated venous pressure would cause a gross distension of veins in the legs, or even damage to tissues due to a lack of oxygen and nutrients.
Apart from conservative measures with postural advice and elastic stockings, surgery would be useful in patients with severe symptoms. Surgery is usually in the form of superficial vein surgery with sapheno-femoral flush ligation, stripping of long saphenous vein with avulsion of varicosity. Injection sclerotherapy may be performed in addition. Closure of long saphenous vein with radiofrequency ablation or laser device are newly developed treatment to replace sapheno-femoral junction ligation and stripping of long saphenous vein. Both radiofrequency ablation and laser are minimally invasive procedure which allows earlier return to work. Their long term efficacy, however, need further evaluation. In patients with advanced CVI, subfascial endoscopic perforator surgery (SEPS) may be helpful.

Varicose veins. Swollen veins caused by incompetent valves. Valves are most susceptible to damage during pregnancy or long hours of standing.