Contact Information
| Telephone: | (852) 2255 4389 |
| Fax: | (852) 2872 8425 |
Activities and Services
The Division of Colorectal Surgery is responsible for the management of patients with benign and malignant diseases of the colon, rectum, anus, small intestine and appendix. With expertise in general surgery and advanced laparoscopic skills, the Division also takes care of patients with abdominal wall hernias, both in elective and emergency settings.
Strengths and Developments
Colorectal Cancer
A multidisciplinary approach with an emphasis on minimally invasive surgery is adopted by the Division in the management of colorectal cancer. Biweekly Multidisciplinary Treatment meetings with clinical oncologists, medical oncologists, radiologists, stoma nurses, and colorectal nurses are held to discuss individual patients to offer the best treatment.

Multi-disciplinary treatment meeting for colorectal malignancy
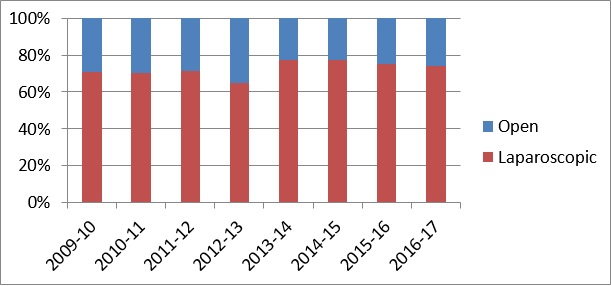
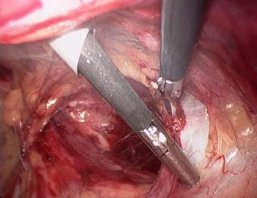
Being a tertiary referral centre, the Division manages a high percentage of patients with advanced or recurrent diseases and low rectal cancer. The specialists of the Division are capable of different approaches in the management of rectal cancer, with the objectives of sphincter preservation and a low recurrence rate. Total mesorectal resection for mid- and low-rectal cancer has been adopted as the standard surgical technique in the treatment of mid and distal rectal cancer since 1993. Currently, total mesorectal excision is regularly performed with either robotic-assisted approach or laparoscopic approach. Transanal total mesorectal excision was first performed in 2014 and is now mainly used for ultra-low rectal cancers. The sphincter-saving rate is over 90% for all mid and distal rectal cancers. The local recurrence rate for patients with low anterior resection has been maintained at around 7%.

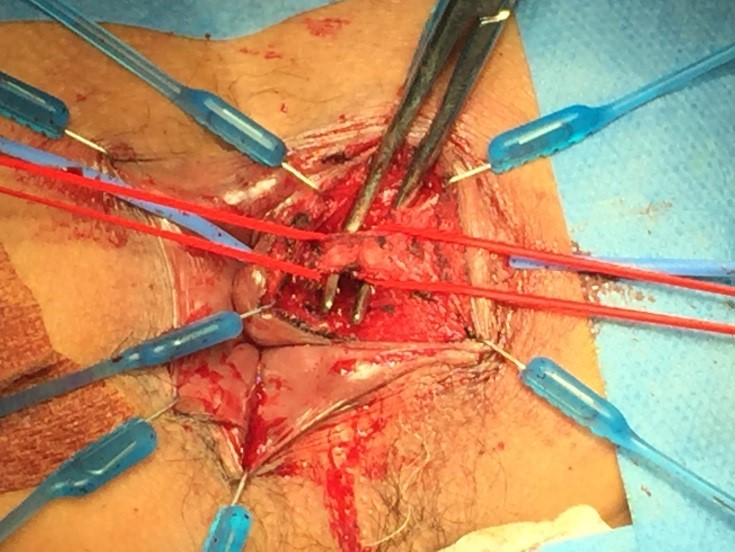
Cytoreduction surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) for a patient with pseudomyxoma peritonei
A protocol for enhanced recovery after surgery (ERAS) has been developed for our patients with elective colorectal resection. The aim is to standardize the treatments for postoperative patients so that more efficient and systematic patient care can be provided and hopefully the length of hospital stay can be shortened. This, together with the minimally invasive approach, has improved the postoperative outcome and shortened the hospital stay.
Inflammatory Bowel Disease
The incidence of inflammatory bowel disease (IBD) is lower in Hong Kong compared with Western countries. The Division works closely with gastroenterologists in the management of these patients. A joint clinic with the gastroenterologist is being held weekly to see patients with IBD. Complex procedures for Crohn’s disease and ulcerative colitis are regularly performed. With the skills in minimally invasive surgery, most of these procedures are performed with laparoscopy.
Anorectal Surgery
Anorectal diseases, such as haemorrhoids and fistulas, are common in patients presenting to our Clinic. With preoperative imaging, such as endoanal ultrasound or MRI, the Division has experience in performing sphincter-sparing procedures for complicated or recurrent anal fistulas, such as the Ligation of Intersphincteric Tract Ligation (LIFT) procedure or fistuloscope.
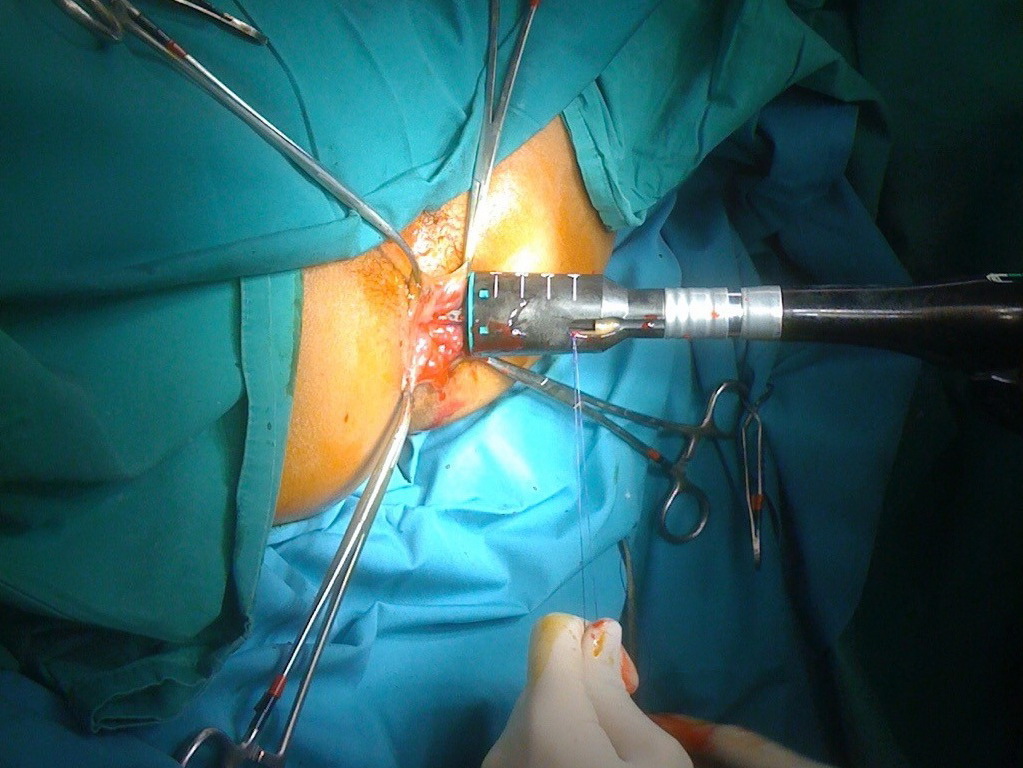
Stapled haemorrhoidectomy
Ligation of Intersphincteric Fistula Tract (LIFT) procedure
Pelvic Floor Disorder
Rectal prolapse is one of the pelvic floor disorders where there is protrusion of the rectum through the anus. Multiple approaches have been used to treat this condition, e.g. the Delorme’s operation, suture rectopexy, etc. Robotic ventral mesh rectopexy has been used in this centre with favourable outcomes.
Peritoneal Surface Malignancies
Endoscopy and Stenting
The Division performs over 3000 colonoscopies each year. In addition to the diagnostic procedures, therapeutic procedures such as colonoscopic polypectomies and insertion of metallic stents are regularly performed. Advanced endoscopic techniques, such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD), are regularly performed.
Anorectal Physiology Laboratory
The anorectal physiology laboratory was established in 1995 to provide objective investigations (such as colonic transit study, 3D endorectal/endoanal ultrasound and high-resolution anorectal manometry) for patients with functional bowel disorders. Endorectal ultrasound helps in the accurate staging of patients with rectal tumour, and endoanal ultrasound could help in managing the complicated anal fistulas or sphincter injury. These then allow the most appropriate treatment to be offered. Anorectal manometry could assess the sphincter function after rectal resection and bowel training can be considered accordingly.
Hernia Surgery
Hernia surgery has evolved rapidly in recent years and is a field of continuous development and research. The Division, together with the staff of Tung Wah Hospital, manages patients with abdominal wall hernias. A clinic catering to new cases of abdominal wall hernias was set up in 2007 in Queen Mary Hospital. Emphasis is put on laparoscopic repair and continuous research in the types of prosthetic mesh and the technique of extraperitoneal repair of groin hernia is underway. Moreover, incisional hernias are now mostly repaired with the laparoscopic approach to reduce surgical trauma.
Needleoscopic Total Extra-Peritoneal (TEP) Hernioplasty with 3mm instruments

Use of Intra-Peritoneal On-Lay Mesh (IPOM) for Incisional Hernia Repair
Colorectal Surgery
Division Activities
| Clinic | Time |
|---|---|
| Colorectal Clinic, S6, QMH |
Monday (a.m.) Wednesday (a.m. & p.m.) Friday (p.m.) |
| Comprehensive Joint Colorectal Cancer Clinic (With Department of Clinical Oncology) |
Wednesday (p.m.) |
| Inflammatory Bowel Disease Clinic (With Division of Gastroenterology Department of Medicine) |
Monday (p.m.) |
| Bowel Continence Clinic | Thursday (a.m.) (every 1st week) |
| Hernia Clinic, S6, QMH | Wednesday (a.m.) |
| Hernia Clinic, TWH | Friday (p.m.) |
| Direct Access PR Bleeding Clinic, TWH | Monday (p.m.) Wednesday (p.m.) Friday (p.m.) |
| Colorectal Clinic for Private Patients Tel: (852) 2255 4293 |
|
| Operating day | Monday: TWH Tuesday: QMH Thursday: QMH Friday: QMH (Alternate week) |
| Endoscopy sessions | Monday (p.m.) Tuesday (p.m.) Wednesday (p.m.) Thursday (p.m.) |
Division Chief
Professor Dominic Chi-Chung FOO傅志聰
Clinical Associate Professor
- MBBS, MS(HK), FRCSEd, FCSHK, FHKAM(Surgery)
| (852) 2255 4389 | |
| ccfoo@hku.hk | |
| HKU Scholar Hub |
Staff List
| Name | Title | Position | Staff types | Telephone | |
|---|---|---|---|---|---|
| Dr. Rockson WEI 韋樂申 |
Division member | Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 4389 | rwei@hku.hk |
| Dr. Hok-Kwok CHOI 蔡學國 |
Division member | Associate Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 4389 |
surgery@hku.hk |
| Dr. Felix Che-Lok CHOW 周祉樂 |
Division member | Associate Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 4389 |
surgery@hku.hk |
| Dr. Alvin Pui-Wai SIU 蕭涪鍏 |
Division member | Associate Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 4389 |
surgery@hku.hk |
| Dr. Pak-Chiu WONG 黃柏釗 |
Division member | Associate Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 4389 |
surgery@hku.hk |
| Professor Victor KUNG 龔滙昇 |
Division member | Clinical Assistant Professor | Academic Staff | (852) 2255 4389 | surgery@hku.hk |
| Dr. Fred Chi-Wai LUI 雷梓維 |
Division member | Resident (Specialist) / Honorary Clinical Tutor | Hospital Authority staff | (852) 2255 4389 | surgery@hku.hk |