Neurosurgery


Contact Information
| Telephone: | (852) 2255 3368 |
| Fax: | (852) 2818 4350 |
Scope and Service
The Division of Neurosurgery is committed to providing the highest level of care to patients with neurosurgical conditions. In addition to offering a comprehensive neurosurgical service to in-patients at Queen Mary Hospital and at a general neurosurgical clinic, the Division also operates other subspecialty neurosurgical clinics, including the Paediatric Neurosurgical Clinic, the Neurovascular Clinic, the Movement Disorder Clinic, the Joint Epilepsy Clinic and the Joint Brain Tumour Clinic at Queen Mary Hospital. A Neuro-rehabilitation Clinic takes place at the MacLehose Medical Rehabilitation Centre. Apart from clinical service, the Division also commits to combine clinical neuroscience from various specialties and research outputs to maximize the standard of care.
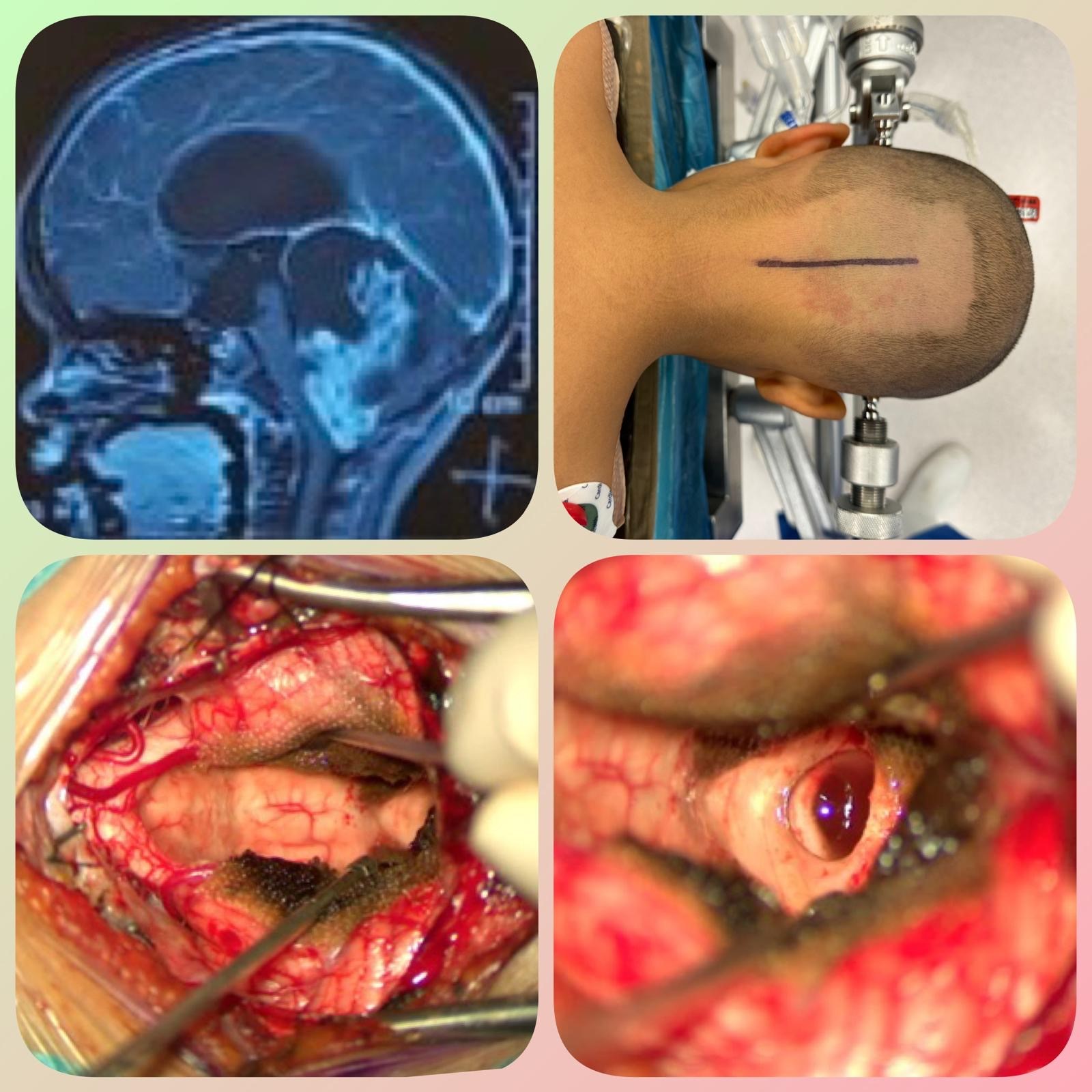
Brain and spine tumour
Our Neuro-oncology service is dedicated to the comprehensive management of brain, spinal cord and head and neck tumours. The majority of brain tumours treated at our division are brain metastasis, malignant glioma and meningioma. We worked closely with clinical oncologists in the Joint Brain Tumour clinic to offer tailored multi-modality treatment that combined surgery, LINAC-based stereotactic radiosurgery, chemotherapy and targeted therapy. To achieve maximum safety resection, awake craniotomy was employed in glioma surgery. Through a patient-centric approach and the integration of innovative therapies e.g. Tumour Treating Field, the Neuro-oncology service at Queen Mary Hospital strives to deliver the best possible care and improve the quality of life for individuals diagnosed with these challenging neurological conditions.
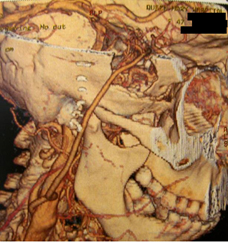
Skull base surgery
The majority of skull base tumours treated at our division are meningioma, chordoma and malignant head and neck tumours. We employed both open and expanded endonasal approaches to minimize morbidity while achieving maximal resection. The expanded endonasal approach provides a direct route to attack skull base tumour and avoid brain retraction during open approach.
In addition to the development of endoscopic transsphenoidal surgery for pituitary tumour in the last decade, our division has also pioneered the simultaneous combined transcranial-transsphenoidal approach to giant pituitary adenoma. This approach has enabled us to achieve complete resection of large pituitary tumours safely in a single setting which previously would require two separate procedures.
We work closely with the Division of Head and Neck Surgery, and the Division of Plastic and Reconstruction Surgery in treating skull base tumours and we have acquired extensive experience in craniofacial resection for anterior skull base lesions such as olfactory neuroblastoma and recurrent head and neck cancer.


Neurovascular surgery
a) Endovascular
The Vascular Neurosurgery team receives tertiary referrals for the management of complex cerebrovascular disorders in Hong Kong and Macau. The team of highly skilled neurosurgeons, neurologists, and interventional radiologists collaborate seamlessly to provide cutting-edge treatment options. The team specializes in open surgical and endovascular management of conditions such as cerebral aneurysms, intra and extra-cranial carotid and vertebral artery disease, arteriovenous malformations, dural arteriovenous fistulas, MMA embolization for chronic subdural hematomas and stroke. Being the first neurosurgery center in Hong Kong to provide 24 hour intra-arterial thrombectomy service, the team aims to continue to deliver efficient and effective care, minimizing risks and improving patient outcomes and positioning ourselves as a premier destination for vascular neurosurgical care in the region.

Thrombectomy:
A 24/7 intra-arterial mechanical thrombectomy service for patients with acute ischaemic stroke has been operational at Queen Mary Hospital since 2018. As of October 2024, over 460 patients have received mechanical thrombectomy, achieving promising results that are compatible with international standards. Further research presented in 2024 indicates that more than 30% of acute ischaemic stroke patients who received endovascular treatment beyond six hours from symptom onset would be able to achieve favourable clinical outcomes.
Eligibility for Mechanical Thrombectomy:
- Ischemic stroke due to large vessel occlusion
- Age 18 or older
- NIH Stroke Score above 6/42
- Satisfactory premorbid functional status
- CT Brain shows no extensive brain infarct
- Onset within 6 hours (if uncertain or onset is between 6-24 hours, advanced imaging will be used)
mRS graph:

Results of Clinical Outcome:
| Within 6 hours from onset | Beyond 6 hours from onset | |
| TICI 2b/3 (%) | 93% | 93% |
| 3 months mRS 0-2 (%) | 43% | 36% |
*TICI score = thrombolysis in cerebral infarction, mRS = Modified Rankin Score
HKUMed Press conference on 14 May, 2024
News Coverage:
1. i-CABLE
2. RTHK
4. TVB
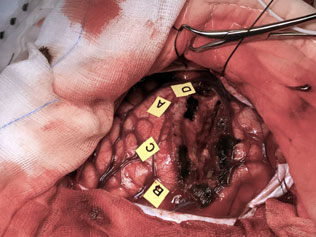
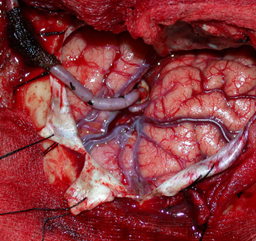
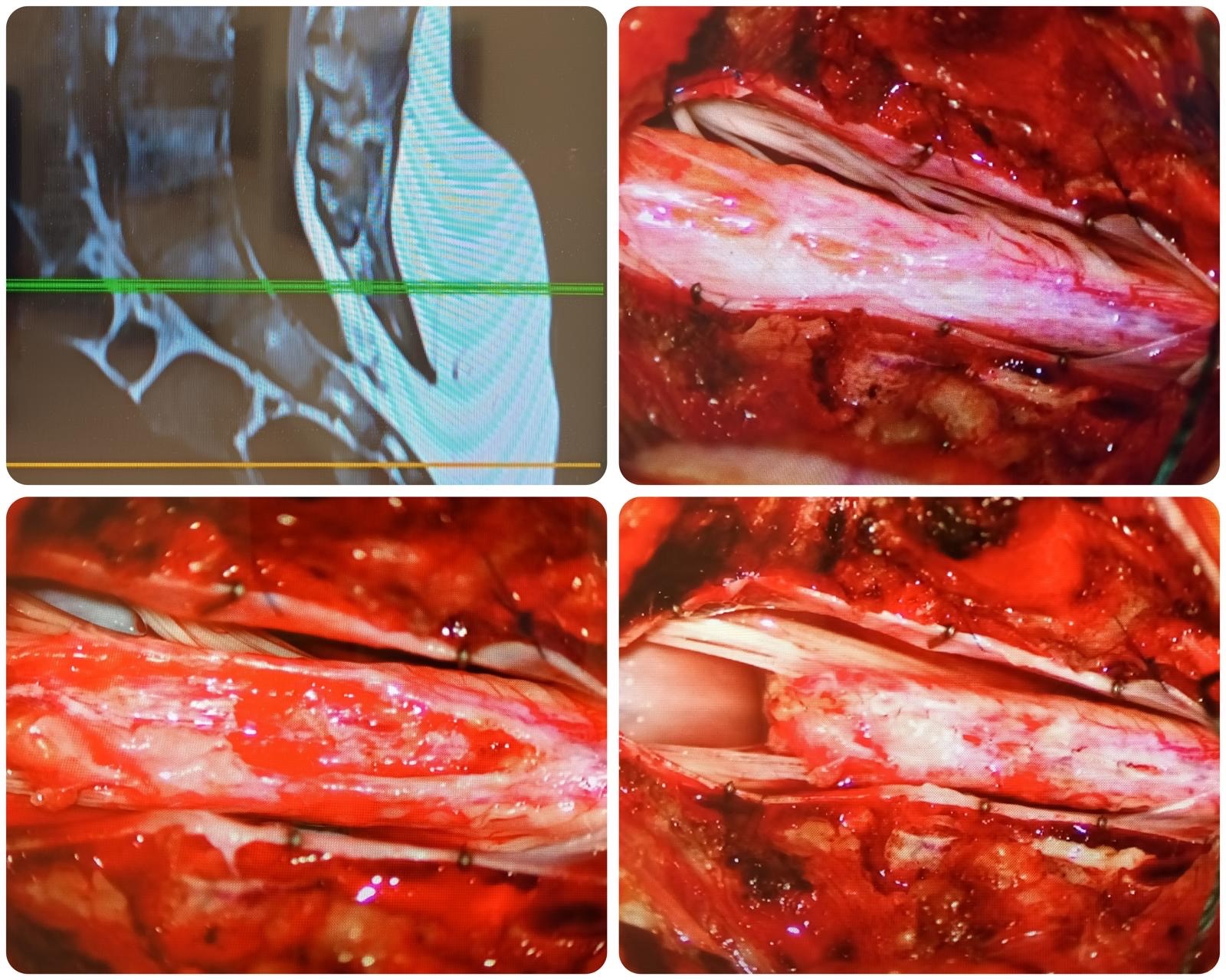
b) Bypass
Endovascular intervention has revolutionarized the treatment of neurovascular diseases in recent years. These include embolization of cerebral aneurysms, arteriovenous malformation, dural arteriovenous fistula, as well as preoperative embolization of brain tumors.
Our centre has pioneered the extracranial-intracranial (EC-IC) bypass procedure in Hong Kong which is a major break-through for cerebral revascularization in the treatment of aneurysm not amendable to endovascular embolization or conventional clipping (e.g., giant aneurysms and radiation-induced carotid artery aneurysms.). We also regularly perform superficial temporal artery-middle cerebral artery (STA-MCA) bypass procedure for symptomatic MoyaMoya disease patients to improve their quality of life and reduce complications development.
 |
 |
Functional neurosurgery
Movement disorders such as Parkinson's disease, dystonia and Tourette syndrome refractory to medical therapy are treated at our unit with deep brain stimulation (DBS) surgery. We are one of the 3 designated centres in Hong Kong performing DBS and performed the first DBS on Tourette syndrome patient in Hong Kong. Queen Mary Hospital is also one of the referral centres for MRI guided focused Ultrasound (MRgFUS) therapy treatment of conditions such as essential tremor.
Epilepsy surgery: We perform various types of surgical procedures for refractory epilepsy including hippocampectomy, resection of epileptic focus, vagal nerve stimulation (VNS) implantation, as well as stereotactic electroencephalogram (SEEG) for surgical planning. We also have the facility to perform DBS for epilepsy. Since 2024, we have acquired the Robotic Surgical Assistant (ROSA), the first station in Hong Kong, for better and more efficient SEEG and other surgical planning. This robotic surgery is also particularly useful for precise tumour biopsy and other surgical planning.
Various pain conditions are treated at our hospital in conjunction with our anaesthetic pain colleagues. Trigeminal neuralgia can be managed by microvascular decompression surgery or radiofrequency ablation (RFA) at our institution. We also manage other chronic pain syndrome such as failed back with implantations of spinal cord stimulators (SCS).
In collaboration with the oncology team, we also perform regular radiosurgery treatments for various kinds of tumours and arteriovenous malformations for patients.


Paediatric neurosurgery
The Paediatric Neurosurgery team in Queen Mary Hospital mainly operates at Hong Kong Children's Hospital, specializing in the management of complex neurosurgical conditions in children. The team’s expertise lies in the surgical treatment of brain and spinal tumours, Chiari malformations, tethered cord syndromes, craniosynostosis and hydrocephalus etc. With a multidisciplinary approach, the team of neurosurgeons, paediatric oncologists, neurologists, and anaesthesiologists work closely together to deliver comprehensive care. Recent advancements have also led to the expansion of the team's capabilities in epilepsy surgery, utilizing cutting-edge techniques and technologies. By fostering strong interdepartmental collaboration, the Paediatric Neurosurgery team is committed to providing world-class neurosurgical care and improving outcomes for our young patients.
Book chapter
Current Practice and New Developments in Trauma
Advances in Electroencephalography and Brain Connectome: Neuroimaging for Epilepsy Diagnosis and Management
By Lau Sau Ning Sarah, Cheng King Fai Kevin and Grace Ho
IntechOpen
Transcranial Approach to Cavernous Sinus and Middle Cranial Fossa
Cheng, King Fai Kevin ; Lui, Wai Man
Singapore: Springer Nature Singapore
Orbital Apex and Periorbital Skull Base Diseases, p.165-173
Research
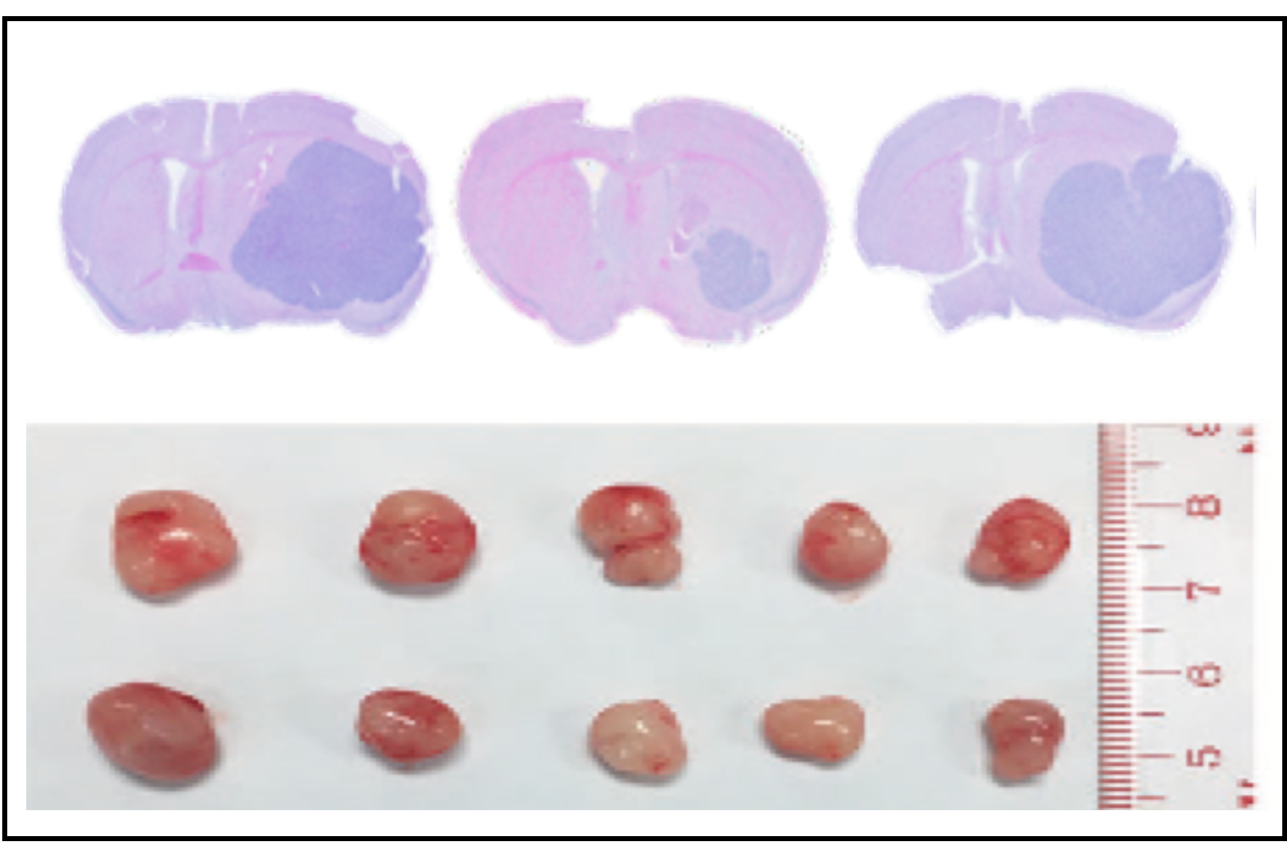
Our laboratory works in translational research focus on neurooncology (e.g., glioblastoma chemoresistance), stroke and neurotrauma (e.g., peri-operative adjunctive neuroprotection), and biomedical engineering (e.g., computerized fluid dynamics). We emphasize the development of novel therapeutic approaches and multidisciplinary collaborations in neuroscience. Our clinical studies focus on skull base surgery, neuroendoscopy, cerebral revascularization and endovascular treatment.
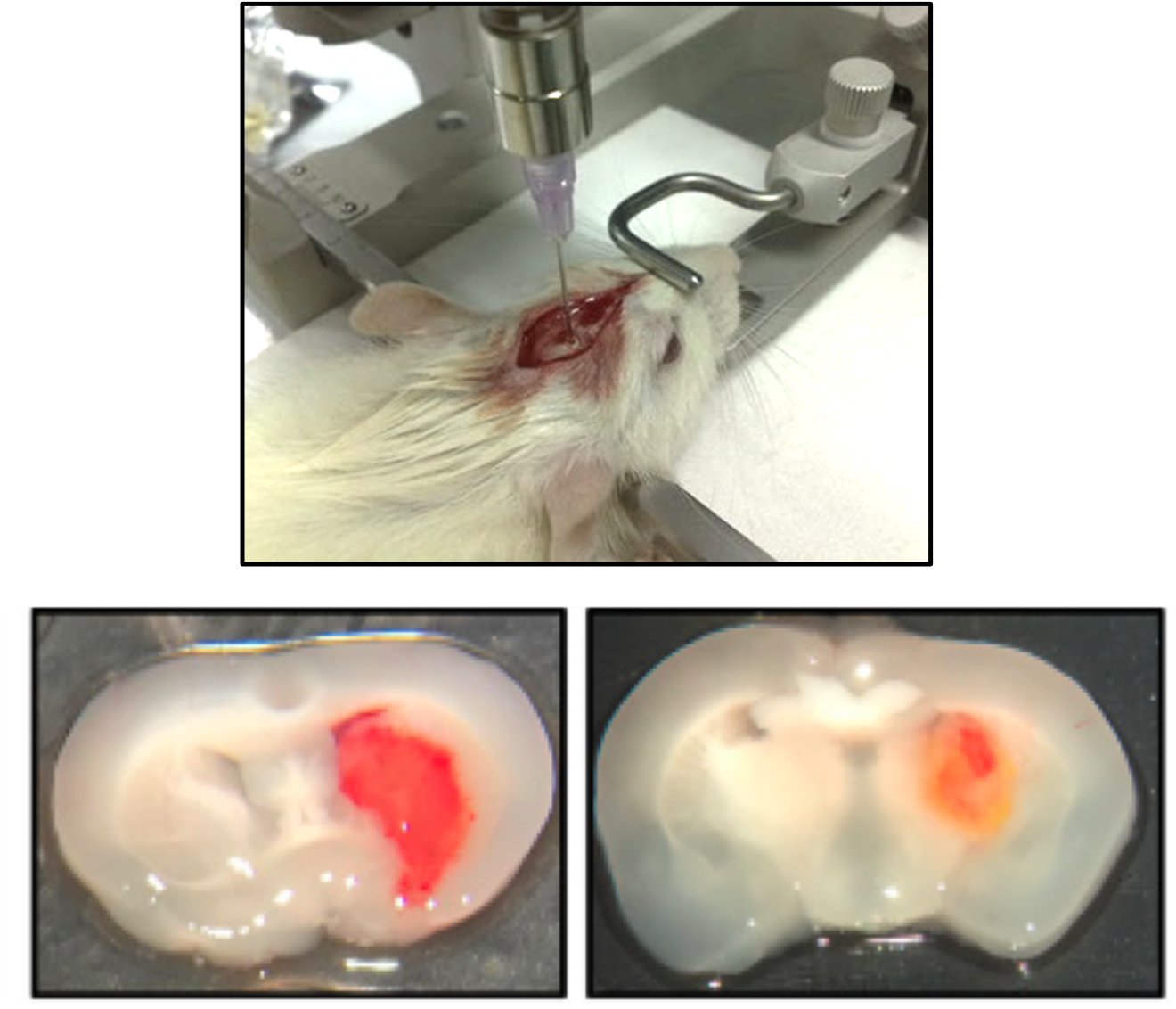
Publications
- Kiang KM, Zhang P, Li N, Zhu Z, Jin L, Leung GK. Loss of cytoskeleton protein ADD3 promotes tumor growth and angiogenesis in glioblastoma multiforme. Cancer Lett 2020; 474:118-26.
- Li N, Yao M, Liu J, Zhu Z, Lam T, Zhang P, Kiang KM, Leung GK. Vitamin D promotes remyelination by suppressing c-Myc and inducing oligodendrocyte precursor cell differentiation after traumatic spinal cord injury. Int J Bio Sci 2022: doi:10.7150/ijbs.73673
- Liu J, Li N, Zhu Z, Kiang KM, Ng ACK, Dong CM, Leung GK. Vitamin D enhances hematoma clearance and neurologic recovery in intracerebral hemorrhage. Stroke 2022;53(6):2058-2068.
- Zhu Z, Kiang KM, Li N, Liu J, Zhang P, Jin L, He X, Zhang S, Leung GK. Folate enzyme MTHFD2 links one-carbon metabolism to unfolded protein response in glioblastoma. Cancer Lett 2022:549;215903.
- Kiang KM, Tang W, Song Q, Liu J, Li N, Lam T, Shum Ho, Zhu Z, Leung GK. Targeting unfolded protein response using albumin-encapsulated nanoparticles attenuates temozolomide resistance in glioblastoma. Brit J Cancer 2023:128;1955-1963.
We also collaborate with other local and overseas investigators in clinical trial and in the development of advanced diagnostics and therapeutics related to neuroscience.
- Liu Y, Leong ATL, Zhao Y, Xiao L, Mak HKF, Tsang ACO, Lau GKK, Leung GKK, Wu EX. A low-cost and shielding-free ultra-low-field brain MRI scanner. Nat Commun 2021;12:7238.
- Choudhury A, Magil ST, Eaton CD, Prage BC, Chen WC, Cady MA, Seo K, Lucas CG, Casey-Clyde TJ, Vasudevan HN, Liu SJ, Villanueva-Meyer JE, Lam T, Pu JK, Li L, Leung GK, Swaney DL, Zhang MY, ChanJW, Qiu Z, Martin MV, Susko MS, Braunstein SE, Bush EAO, Schulte J, Butowski N, Sneed PK, Berger MS, Krogan NJ, Perry A, Phillips JJ, Solomon DA, Costello JF, McDermott MC, Rich JN, Raleigh DR.Meningioma DNA methylation grouping reveals biologic drivers and therapeutic vulnerabilities. Nat Genet 2022;54(5):649-659.
- Man C, Lau V, Su S, Zhao Y, Xiao L, Ding Y, Leung GKK, Leong ATL, Wu E. Deep learning enabled fast 3D brain MRI at 0.055 Tesla. Sci Advances 2023;9(38):edai9367.
- Teo K, Fong S, Leung WCY, Leung IYH, Wong Y, Choi OMY, Yam KK, Lo RCN, Cheung RTF, Ho S, Tsang ACO, Leung GKK, Chan KH, Lau GKK. Location-specific hematoma volume cut-off and clinical outcomes in intracerebral hemorrhage. Stroke 2023:54;1538-1557.
- Chen WC, Choudhury A, Young MW, Polley MC, LucasCG, MirchiaK, MaasSLN, Suwala A, Won, Bayley JC, Harmanci AS, Klisch T, NguyenMP, Vasudevan HN, Yu TJ, Bhave V, Lam TC, Pu JK, Li L, Leung GK, Chan JW, Perlow HK, Palmer JD, Haberler C, Berghoff AS, Preusser M, Nicolaides TP, Mawrin C, Agnihotri S, Resnick A, Rood B, Chew J, Young JS, Boreta L, Braunstein SE, Schulte J, Butowski N, Santagata S, Spetzler D, Bush NAO, Villanueva-Meyer JE, Solomon DA, Pugh SL, Mehta MP, Sneed PK, Berger MS, Horbinski CM, McDermott MW, Perry A, Bi WL, Patel AL, Sahm F, Magill ST, Raleigh DR. Targeted gene expression profiling predicts meningioma outcomes and radiotherapy responses. Nat Medicine 2023 (in press).
Division Chief
Dr. Kevin King-Fai CHENG 鄭璟暉
Consultant
Honorary Clinical Associate Professor
- MBBS(HK), FRCSEd(SN), FCSHK, FHKAM(Surgery)
| (852) 2255 3368 | |
| ckf414@ha.org.hk |
Staff List
| Name | Title | Position | Staff types | Telephone | |
|---|---|---|---|---|---|
| Dr. Wai-Man LUI 呂偉文 |
Division member | Consultant / Honorary Clinical Associate Professor | Hospital Authority staff | (852) 2255 3368 | luiwm1@ha.org.hk |
| Professor Gilberto Ka-Kit LEUNG 梁嘉傑 |
Division member | Clinical Professor | Academic staff | (852) 2255 5618 | gilberto@hku.hk |
| Dr. Wilson Wai-Shing HO 何偉成 |
Division member | Consultant / Honorary Clinical Associate Professor | HKU-SZ Hospital staff | (852) 2255 3324 | howsw@hku.hk |
| Dr. Lai-Fung LI 李禮峰 |
Division member | Consultant / Honorary Clinical Associate Professor | Hospital Authority staff | (852) 2255 3368 | llfrandom@gmail.com |
| Dr. Benedict Beng-Teck TAW 杜明德 |
Division member | Consultant / Honorary Clinical Associate Professor | Hospital Authority staff | (852) 2255 3368 | tbt061@ha.org.hk |
| Dr. James Tin-Fong ZHUANG 莊天放 |
Division member | Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 3368 | tfzhuang@yahoo.com.hk |
| Dr. Sarah Sau-Ning LAU 劉秀寧 |
Division member | Associate Consultant / Honorary Clinical Assistant Professor | Hospital Authority staff | (852) 2255 3368 | lsn617@ha.org.hk |
| Dr. Benjamin Wai-Yue LO 羅懷宇 |
Division member | Associate Consultant | Hospital Authority staff | (852) 2255 3368 | lbw606@ha.org.hk |