Cardiothoracic Surgery
Contact Information
| Contact phone: | (852) 2255 5877 |
| Fax: | (852) 2553 3436 |
History
During the 1950s to 1960s, thoracic surgery in Hong Kong was mostly confined to thoracoplasty for extensive pulmonary tuberculosis and lung resections. In 1964, when Prof. G.B. Ong was appointed as the Chair of Surgery at the University of Hong Kong, the Departments of Medicine and Surgery at the University, in response to the increasing need for open heart surgery locally, along with the Hong Kong Government and the Hong Kong Anti-Tuberculosis Association (HKATA), initiated the introduction of open-heart surgery to Hong Kong.
Timeline and important milestones
1964
- Department of Surgery took over the Thoracic Surgical Units at The Grantham Hospital (GH) in 1966.
11th December, 1964
- The first open-heart operation in Hong Kong was performed by Professor GB Ong at Queen Mary Hospital (QMH) on a female patient with patent ductus arteriosis, pulmonary valve stenosis and atrial septal defect (ASD) under hypothermic circulatory arrest.
1966-69
- Drs KH Kwong and John Leung underwent open-heart surgery training overseas. Practise of cardiopulmonary bypass in animals started at GH in 1967/68.
30th July, 1968
- The first open heart surgery performed in The Grantham Hospital. Dr. KH Kwong assisted Dr. Lester Bryant, an American cardiac surgeon from Lexington, Kentucky, to close an ASD in a 17-year-old girl with cardiopulmonary bypass.
16th September, 1975
- The first neonatal survivor in Hong Kong after open heart surgery: a 2-month-old girl who underwent VSD & ASD closure.
1978
- Cardiac catherization laboratory was established at GH.
1992
- The first heart transplantation in Hong Kong.
1995
- The first single lung transplantation and the first heart-lung transplantation were performed.
1996
- Off pump coronary artery bypass grafting and minimally invasive direct coronary artery bypass (MIDCAB) introduced.
1997
- The first double-lung transplantation was performed.
2000
- Extracoporeal membrane oxygenation support for paediatric patients started.
2004
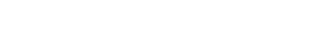
- The first successful implantation of the Left Ventricular Assist Device (LVAD) in Hong Kong using the Berlin Heart Device in a 7-year-old boy with acute fulminant myocarditis.
2006
- First minimally invasive mitral valve repair operation.
2008
- The Cardiothoracic Surgical Unit and Paediatric Cardiac Unit at Grantham Hospital (GH) was relocated to Queen Mary Hospital, providing state-of the-art multidisciplinary care to patients in three OT suites, 16 cardiothoracic ICU beds and 60+ step-down beds.
2009
- First Paediatric heart transplantation in Hong Kong.
2010
- Successful implantation of the first fully implantable LVAD (Heartmate II) in a 30-year-old adult with end-stage dilated cardiomyopathy, kick starting the LVAD program in Queen Mary Hospital.
- First Heart-liver transplantation in Hong Kong.
2011
- First adult ventricular assist device (CentriMag) implantation in supporting right and left heart for patient with acute ventricular failure.
2012
- First transfemoral TAVI operation performed.
- First “QMH Cardiac Surgery Biennial Report 2010-2011” on the outcomes of adult cardiac surgery published.
2013
- First transapical TAVI operation performed.
- First LVAD patient bridged to heart transplant.
- First Paediatric patient with Berlin Heart bridged to heart transplant.
2014 2017 2018 2019 2020 2021 2023 2024

Department Photo
LVAD
Activites and Services
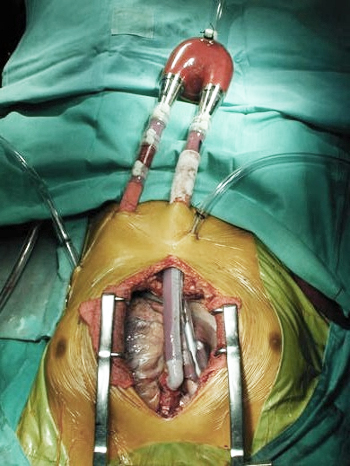
The service was originally established in GH and was relocated to QMH on 25 July 2008.The Division of Cardiothoracic Surgery is Hong Kong's largest tertiary referral center for heart and lung diseases, receiving elective and emergency referrals from all public and private hospitals, as well as from Macau and nearby regions. Cross-disciplinary support is provided to other units at Queen Mary Hospital. It is the sole referral center in Hong Kong for adult congenital heart disease, organ transplantation, and mechanical circulatory support. Adult Cardiac Surgery Services Queen Mary Hospital is the leading provider of open-heart surgeries in Hong Kong, performing over 600 procedures annually. It specializes in coronary artery bypass, heart valve, arrhythmia, transplantation, ventricular assist devices, and aortic surgeries. The Division offers a wide array of procedures, including open-heart, minimally invasive, catheter-based and endovascular procedures. The Division performs a range of coronary artery surgery, from complex to minimally invasive CABG such as Off-Pump Coronary Artery Bypass Grafting (OPCABG) and Minimally Invasive Direct Coronary Artery Bypass Grafting (MIDCABG). The Division was an early adopter in Asia of endoscopic vein harvesting (EVH) and endoscopic radial artery harvesting (ERAH) techniques for coronary artery bypass grafting which are now routinely used to improve patient outcomes. The Division treats complex heart valve disease using both open-heart and minimally invasive techniques. Minimally invasive techniques allow for interventions in patient’s high risk for open procedures and allow quick recovery. Beating heart valve repair and replacement include Neochord mitral valve repair, transcatheter aortic valve replacement (including J valve for aortic regurgitation), mitral valve replacement, tricuspid valve replacement and pulmonary valve replacement. The Division became the first in Asia to adopt NeoChord DS 1000 system for mitral valve repair technique in 2018. The Division routinely offers surgical radiofrequency ablation for atrial fibrillation in patients undergoing open heart surgeries. It is the first center in Asia to offer hybrid surgical-catheter ablation to patients with hard-to-treat atrial fibrillation. This innovative approach involves a collaborative effort between cardiologists and cardiac surgeons, resulting in improved outcomes and a positive impact on the quality of life for patients. Adult congenital heart surgery The Division was the sole paediatric cardiac surgical center in Hong Kong until October 2020, when the service transferred to Hong Kong Children's Hospital. It now focuses on Adult Congenital Cardiac Surgical Services, specializing in treating all forms of adult congenital heart disease, including aortic stenosis and bicuspid aortic valve, atrioventricular canal defects, coarctation of aorta, conduit revisions, Ebstein’s anomaly, ostium primum and secundum atrial septal defects including patent foramen ovale, patent ductus arteriosus, pulmonary stenosis and regurgitation, pulmonary atresia, single ventricle, transposition of great arteries, Tetralogy of Fallot, anomalous coronary artery, and ventricular septal defects. Heart and Lung Transplantation The Division has been the exclusive provider of intra-thoracic organ transplantation in Hong Kong since 1992. To date, over 250 heart transplants and 100 lung transplants have been successfully performed. In 2020, the Organ Care System (OCS) was implemented for donor hearts that did not meet standard acceptance criteria for transplantation. This innovative approach allows for the potential addition of 3 to 5 extra hearts for transplantation each year without compromising early outcomes. The division is expanding the availability of suitable donor lungs through Ex Vivo Lung Perfusion (EVLP). Surgeons have undergone training in EVLP techniques using animal models and are actively working toward implementing this method in human patients. Mechanical circulatory support and LVAD program In 2004, Queen Mary Hospital achieved a milestone by performing Hong Kong's first Left Ventricular Assist Device (LVAD) implantation using the Berlin Heart Device on a 7-year-old boy with acute fulminant myocarditis. The HeartMate II was introduced in 2010, followed by the HeartMate III in 2017. To date, 205 LVADs have been implanted. A dedicated LVAD team—comprising cardiac surgeons, anesthetists, cardiologists, nurses, and allied health professionals—provides personalized, comprehensive support throughout each patient's LVAD journey. The LVAD nursing team received the Asia Hospital Management Award in 2012 and the Outstanding Teams Award from the Hong Kong West Cluster & Queen Mary Hospital in 2014. The Division offers Extracorporeal Membrane Oxygenation (ECMO) support for adults with critical lung or heart conditions, supported by specialized trained surgeons and nurses. To date, over 500 patients have received ECMO support. Aortic surgery The Division provides a comprehensive array of treatments for thoracic aortic disease, employing advanced open, endovascular, and hybrid techniques. It addresses conditions such as thoracic aortic aneurysms, acute and chronic dissections, and Marfan’s syndrome. Each year, the team performs over 200 aortic surgeries, including procedures for the aortic root, arch, frozen elephant trunk, descending aorta, and thoracoabdominal aorta. Through a multidisciplinary approach, they offer minimally invasive surgeries for complex pathologies of the aortic arch and descending thoracic aorta, including TEVAR. Thoracic Surgery Services The division specializes in treating a wide range of conditions affecting the lungs, esophagus, mediastinum, diaphragm, and chest wall performing over 500 thoracic procedures annually. Surgical expertise encompasses various procedures, with the most commonly performed operations including lobectomy for lung cancer, thymectomy for thymic tumors or myasthenia gravis and lung transplantation. Surgeons perform all minimally invasive thoracic surgical procedures, as well as traditional open procedures. Minimally invasive thoracic surgical procedures include thoracoscopy, video-assisted thoracic surgery (VATS), and robotic thoracic surgery. Monitoring clinical outcomes For quality assurance and monitoring of clinical outcomes, the Division collaborates with other centers in Hong Kong to collect prospective clinical data using the Dendrite Clinical System’s Cardiac Surgery registry. Additionally, the Division maintains transparency and accountability by routinely publishing its biennial report, which provides detailed information on its heart surgery activities, including the number of procedures performed and their respective outcomes. Training and Research As part of the Department of Surgery at the University of Hong Kong, the Division is dedicated to training the next generation of surgeons through residency and fellowship programs, alongside organizing continuing medical education conferences and symposia. Funded opportunities for international meetings and support for overseas training are also provided. It initiated the Master of Nursing (MNurs) program in perfusion science in 2019 in collaboration with the School of Nursing to address the shortage of perfusionists in Hong Kong.
Cardiac Surgery Biennial Reports
Cardiac Surgery Biennial Report 2022-2023
Cardiac Surgery Biennial Report 2020-2021
Cardiac Surgery Biennial Report 2018-2019
Staff List
| Name | Title | Position | Staff types | Telephone | |
|---|---|---|---|---|---|
| Dr. Cally Ka-Lai HO 何嘉麗 |
Chief | Chief of Service / Consultant | Hospital Authority staff | (852) 2255 5877 |
hoklc@ha.org.hk |
| Professor Daniel Tai-Leung CHAN 陳泰良 |
Division member | Clinical Associate Professor | Academic staff | (852) 2255 4637 | dc607@hku.hk |
| Professor Michael Kuan-Yew HSIN 辛光耀 |
Division member | Clinical Associate Professor | Academic staff | (852) 2255 4637 |
mkhsin@hku.hk |
| Dr. Oswald Joseph On-Jing LEE 李岸政 |
Division member | Consultant | Hospital Authority staff | (852) 2255 5877 |
loj328@ha.org.hk |
| Dr. Lucius Kwok-Fai LEE 李國暉 |
Division member |
|
Hospital Authority staff | (852) 2255 5877 | lkf322@ha.org.hk |
| Dr. Tsz-Him LING 凌子謙 |
Division member | Consultant | Hospital Authority staff | (852) 2255 5877 |
lth144@ha.org.hk |